With so many opportunities available for experience around training programmes there can be difficult decisions for junior doctors deciding, if, when and how, to best combine their other interests with their medical career. Here, we proudly present Adventure Medic’s Updated Guide to Taking Time Out From UK Training.

More and more UK doctors are opting to take time out of training in order to pursue medical and personal interests all over the world. The number of doctors requesting certificates of good standing (needed to register with an overseas medical council) was 4,804 in 2016 when the GMC last released data on this. According to the Foundation Programme survey, numbers entering speciality training directly from the Foundation Programme have continued to fall with only 37.7% of doctors remaining in training in 2018. A schematic summarising the changes over the last eight years was published by the BMJ (Figure 1). Later career breaks have also become more common, with Health Education England stating that this should be expected and recognised as a normal part of many doctors’ progress. There has been a culture shift with many colleges now actively supporting opportunities around the traditional training pathway.
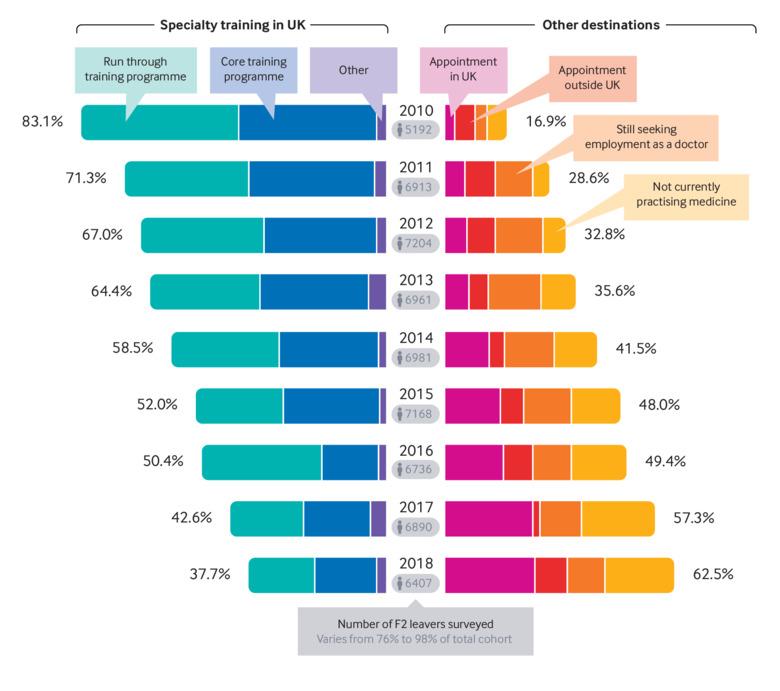
Moberly T, Stahl-Timmins W. BMJ 2019; 364: l842
Here at Adventure Medic, we feel passionately about the personal and professional benefits to be gained by taking time out from medical training in the UK – whether your motivation is to broaden your clinical exposure, to experience developing world medicine, to resolve specialty or career indecision, to pursue personal interests, or even just to exercise some autonomy over your work and professional development. Not to mention the (very valid) reasons of travel and adventure for their own sakes.
The British Medical Association proposes that the key question to ask yourself is, ‘will you be better equipped at the end of your time out than at the beginning?’. If you’re organised and motivated, it’s very easy to ensure the answer to this question is a firm ‘yes’.
When to take time out?
Before Foundation / Unless there is an opportunity that will not wait, it’s not advisable to delay the move from medical school into Foundation Training. The support of your Medical School during the Foundation Programme application process is invaluable. The transition from student to FY1 is a steep and often daunting learning curve, and one best travelled with the support of your peers. In addition, whilst you have graduated with a medical degree, until you’ve completed your first year of the Foundation Programme, you are only registered in a provisional context by the GMC. In other words, you are not eligible to practice medicine independently or outside your place of supervised employment. If you’re still considering it, information regarding the requirements for time out at this stage can be found on the GMC and UKFP websites.
Between FY1 and FY2 / Some Foundation Schools will support time out between FY1 and FY2, or accredit an FY2 year abroad. If you are interested, it is best to make your enquiries early with your Foundation School Director, as there is considerable variation across schools. In 2019 only Wessex, Severn and Peninsula advertised an allowance for FY2 training abroad. Note that due to Australian immigration laws, you can currently only work in Australia after two years of employment. This makes an FY2 year here impossible unless you hold Australian citizenship. New Zealand and South Africa remain options. See the individual Foundation School pages on the UKFP website for more information.
After FY2 / Probably the most popular time to head away is after completing FY2. At this stage, you have full registration with the GMC, a broad base of general medical skills and you are at a natural break in the job ladder. It’s also a time when many junior doctors experience doubt over choice of specialty (or even over choice of career), so the opportunity to experience medicine in a different context or continent can be invaluable.
After Core Training / For non run-through specialties such as Core Medical, Anaesthesia and Surgery, completion of the CT2 year is also a natural break in the system, and many doctors choose to divert at this point, with the advantage of another couple of years experience under their belt.
In Specialty Training / Most specialty training programmes enable Out Of Programme Experience (OOPE), Out of Programme Training (OOPT), Out of Programme Research (OOPR) and Out of Programme Career Breaks (OOPC). Availability varies by Local Education and Training Board (LETB) and in some specialties OOP is becoming more difficult to get due service provision pressures. Again, if you’re interested, it is worth expressing interest early and enquiring of your Postgraduate Dean before you enrol on a particular programme. You may also have the opportunity to do a fellowship abroad in an area of special interest during your advanced specialty training.
Where to go?
It can seem daunting to know which direction to go in, given that there is a whole world outside. There are lots of wonderful opportunities, and part of the fun is designing your own unique adventure. After all, when else in medicine will you be the master of your own fate? In the meantime though, here is some basic information on some of the routes better travelled to get you started.
Australia / The Australian job market has tightened up somewhat in recent years as word of the glorious sunshine, pay and hours has filtered up to the beleaguered inhabitants of the Northern Hemisphere. However, there are still some jobs to be had. You are eligible to apply if you are a UK citizen and UK graduate, but Australia has explicitly chosen to give priority to Australian and New Zealand candidates over us Brits. Jobs are advertised state by state, and within states there are centralised online application websites. While the design, layout and deadlines vary from state to state, the basic process is the same all over the country. Typically, jobs are posted online from late June to early August. Interviews take place from late August to Mid-September and offers are made by early October. Jobs then start between mid-January and mid-February. A sensible approach is to choose the city or area that appeals and then get a list of all the hospitals in a 20-100 mile radius (depending on location). Call (rather than e-mail) each hospital and try and get through to the medical workforce unit. Follow up your call with an email and your CV. Don’t be discouraged and keep at it. It is also possible to get jobs through the year via ‘unofficial’ pathways, particularly between September and November as people start to resign posts and places free up before the end of the year. Make sure you leave yourself plenty of time as you need to get registered with the AHPRA (Australian Health Practitioner Regulation Agency) to start work and this can take 6 months.
New Zealand / You are eligible to apply to New Zealand if you are a UK citizen and a UK graduate. You can apply for a post as a House Surgeon or a Registrar. House Surgeons are roughly equivalent to FY2’s, but Kiwis may spend several extra years at that grade getting experience in a wide range of specialities. Registrars are equivalent to CT1/ST1 and upwards. As specialty training in New Zealand is typically five years rather than seven, you will be worked quite hard at Registrar level and given somewhat more responsibility. However, it is a great way to get experience. Sometimes UK doctors will start out as House Surgeons and then choose to join the Registrar rota once they have found their feet. Applications for New Zealand are usually in April/May with offers in August for end of November (House Surgeons)/early December (Registrar) starts. Apply direct to hospitals via the RMO Office. After getting an offer, you can then apply for registration with the New Zealand Medical Council, get your visa and indemnity and finally book your flights. If you are going for longer than one year, you will require a medical for the visa, but that can also be done in New Zealand and your visa subsequently extended. Keep all the receipts, as the hospital will reimburse you. For more information on working in NZ, see our guide.
Europe / Given that it is on our doorstep, surprisingly few doctors go to Europe. While language is still the main limitation to crossing the Channel, Brexit has made it harder to do so. There is no longer freedom of movement and your qualification is not automatically transferrable. However, it is still possible! We recommend contacting the relevant country’s regulatory body for advice on obtaining a license to practice. You may need to have your qualification translated and verified by the regulatory body. Once you have the right to practice, you’ll need to apply for a VISA through your chosen country’s embassy. Be aware about different medical systems, indemnities, registration requirements and speciality structures. Finally, in some European countries, there are quite high levels of medical unemployment, so finding a job may be difficult. However, for those with good language skills and a thirst for the Continent, don’t be put off.
North America / Love red tape? Exams? Hard work? Then North America is for you. The BMA provides excellent online guides to working in the USA and Canada which are good places to start. Broadly, the issues are eligibility to work and visas, training requirements, exams and competing with homegrown candidates. For those looking for a short fix, research posts and some fellowships are a good way to spend time working in North American institutions, while avoiding the exams.
Developing World Work / Developing world work can be an immensely satisfying way to consolidate your medical skills and get some love back for being a doctor. Work can either be arranged yourself, or through an organisation or NGO. Different posts will have different professional requirements, and some ask for additional qualifications such as a tropical medicine diploma. Whatever the organisation’s requirements however, you have to satisfy yourself that you are the right person for the job. Consider whether other doctors of similar experience have gone before you, what supervision will be in place, and what the arrangements are regarding salary or expenses. You will likely have to register with the country’s medical council, which can take some time. The best advice for arranging a developing world placement is to start early and be persistent. Please visit our Resources Section for details of some charities and organisations who may be of interest.
Expedition Medicine / Expeditions are a particular passion of ours here at Adventure Medic HQ. In theory, any doctor with a license to practice (i.e. post- Foundation) can go on an expedition and many do. However, there are a number of ways to keep yourself right. First of all, make sure you are up to the job. Get a thorough understanding of the nature of the trip and the participants before accepting, and be honest about your own experience. Expedition docs are subject to the Bolam Test (Hunter vs. Hanley for Scots) – in other words, your actions will be judged against your peers. If you bill yourself as a ‘mountain medicine expert’, expect to be judged against other experts should the worst happen and you end up in court. For your first expedition, it may be good to go with one of the more well-known organisations, such as Raleigh International or Blue Ventures, as they are used to junior doctors. Whoever you go with, make sure that they are clear about the deal that they are offering. Do they include flights? Kit? Indemnity? Expenses in country? A salary/per diem? Be wary of operators who offer you ‘10% off’ off the cost of the trip if you are willing to act as doctor. Often, the cost of kit, indemnity and preparation time will be considerably more than the 10% and may detract from your enjoyment of the expedition. A good way to take the stress out of being an expedition doctor is to go on a course first. There are a number listed in our Resources Section. As well as teaching you some of the skills, courses are also great ways to make contacts in the expedition world. Good luck, and let us know how you get on!
Staying in the UK / Many people choose to take time out of training and remain in the UK. This can be a great choice for those who wish to stay a little closer to home but want a break from or aren’t ready to enter a formal training programme. Ad-hoc locum work can give you flexibility to travel, do additional courses or qualifications or even expedition or voluntary work abroad. Additionally, there is a dizzying array of ‘fellowship’ type posts that have appeared in the last 5 years which offer a fixed term contract with training opportunities and additional perks built in. These can offer fantastic opportunities to gain valuable experience and skills, or to try your hand at specialties that perhaps you didn’t have an opportunity to do previously.
Recruitment Agencies / Recruitment agencies can take a lot of the hassle out of arranging work abroad. However, be aware that they are a bit like budget airlines – they often take you somewhere near to where you want to go. Be very sure where you are being placed. Remember also that agencies make a lot of money for every doctor they place, so you are doing them a favour not the other way around. Drive a good bargain.
Tempted?
Adventure Medic talked to an eclectic bunch of medics who’ve successfully deviated from the straight and narrow at various points in their medical careers. Between them they’ve mountain biked the Simien mountains, lived the dream in New Zealand, dived or sailed off every continent and driven across the African plains. They hope to provide you with encouragement, ideas and inspiration. They’ve also provided us with a wealth of helpful tips including things to consider when taking time out and how to ensure you keep yourself right.
Rich Wain-Hobson
Graduated / Peninsula, 2010
Time out / Three years after F2, 6 months after GP training
What did you do? Drove an old Land Rover from Cornwall to Cape Town (www.cornwalltocapetown.com), supported the world’s first commercial mountain biking expedition to the Simien Mountains in Ethiopia, worked on boats in both Antarctica and the Arctic, worked as a photographer on a trip driving from Ireland to Far Eastern Siberia, travelled independently by horse in Kyrgyzstan, completed a Diploma in Tropical Medicine (DTMH), spent 3 months ski touring in Austria, saw a lot of family and friends… and locumed in Cornwall for money!
Best bits? Planning my own expeditions. Doing it yourself means you learn about all aspects of expeditions, from communications devices through to mechanics (or how to look after a horse!)
Any other adventures along the way? Just the unexpected – friends, opportunities, random acts of extreme kindness. And an overwhelming feeling at the end of it all that there’s more to life than climbing the Greasy Pole.
Any regrets? Not using my DTMH – I waited to go away with MSF for 5 months and it never happened. And worrying too much about a career. Almost everyone I know who’s taken time out has landed the job they wanted when they came home.
What are your plans now? Just got back from a mountain filled year working as a GP in Christchurch, NZ. Time to get stuck back into the NHS, with a trip here and there for sanity, of course!
Becca Jancis
Graduated / Leeds, 2015
Time out / Two years after FY2
What did you do? Worked as a diving and hyperbaric doctor at the Diving Disease Research Centre (DDRC) with time for dive expeditions in Indonesia, supported ultramarathon runners in Kenya and along the Pennine Way in the UK and earnt money to travel and dive while gaining extra ED experience.
Best bits? Having the chance to combine my love of traveling with medicine. This gave me a chance to see how people’s bodies react when they push themselves to the extremes. I had time to travel for prolonged periods of time which would have been impossible in full time training. I was given the opportunity to teach on undergraduate to masters courses and have now set up the expedition dive medicine course.
Any other adventures along the way? Popped over to New Zealand to see my friends who are working out there. This was an awesome opportunity to explore the mountains, swim with dolphins and whale watch. Diving and surfing on the other side of the world was pretty sweet too. I can see why they aren’t all coming back to the UK!
Any regrets? Of course not!
What are your plans now? I’m joining the Navy. Hoping that I have plenty of opportunities for ongoing adventures and ideally lots of diving.
Calum Stannett
Graduated / Edinburgh, 2015
Time out / After FY2, 18 months and still away…
What did you do? Spent a year working in ED as an agency locum in various hospitals around Scotland including Fort William in the Scottish Highlands, did a 5,500km cycle touring trip for three months from the far north of Norway back to Scotland, completed my paragliding qualifications, moved to New Zealand and bought a campervan and have since travelled around NZ exploring as much as possible by foot, bike and wing.
Best bits? Choosing to do agency work gave me huge flexibility and control over my time with the added bonus of being able to tuck away some coin! This allowed me to travel, as well as try a variety of specialties to help me make an informed decision about my next steps. Staying in Scotland also meant I could spend more time with family and friends.
Any other adventures along the way? I spent a week on a guided alpine mountaineering course in the French Alps and 3 weeks bikepacking through the south of Spain. I also finished my ALS instructor training and taught on several courses.
Any regrets? Definitely not!
What are your plans now? I’ve just bought a house in Christchurch, NZ. My main goals are getting the veggie garden pumping and making the most of the paragliding season. I plan to apply for GP training in NZ later this year and will be here for the foreseeable future.
Satti Marwaha
Graduated / Bristol, 2012
Time out / 1 year after FY2, 1 year between ST3 & ST4
What did you do? After FY2 I spent 6 months on a clinical fellowship at Southampton Neuro ICU, volunteered in a rural health clinic on the island of Leyte in the Philippines and travelled in South-East Asia. Suffering more wanderlust, I took a 6-month OOPE post EM ST3 and lived in South Africa on a Health Education England leadership fellowship and then volunteered with a Dutch NGO in Camp Moria Refugee Camp in Greece.
Best bits? Learning to love medicine again in the Philippines. Portfolio and assessment free; it allowed me to focus on the clinical side of medicine and enjoy using my clinical acumen to make decisions in a resource poor setting. A non-clinical role in SA allowed me to work “9-5”. Although this had the benefit of a predictable lifestyle, I learnt that the grass isn’t always greener on the other side and a “9-5” office job is not for everyone. Working alongside refugees to deliver healthcare in Camp Moria.
Any other adventures along the way? Becoming the residential doctor for advice in the community I lived with in the Philippines. Being part of the major incident team when wild fires loomed near the hospital. Not declining adventures because of shifts…
Any Regrets? No. Time out of training and travel will always make you richer (but not in a financial sense..).
What are your plans now? Continuing EM training. Undertaking a Postgraduate Certificate in Global Health Leadership. Planning my next OOPE…
Kirsty Wright
Graduated / Glasgow University, 2008
Time out / 2 years after FY2, 18 months after ST3
What did you do? Career break 1 – worked in New Zealand for 18 months (mainly having adventures), then completed the DTMH in Liverpool before volunteering in Peru with the Vine Trust. Career break 2 – volunteered with AMREF (aeromedical retrieval), Mercy Ships (teaching the WHO Surgical Safety Checklist to local hospitals in Benin), and finally 6 months in Zambia as a Junior Teaching Fellow with the Global Anaesthesia Development Project.
Best bits? Meeting like minded people, combining my love of travel and adventure with medicine, opportunity to work with some incredible people all over the world. But mainly making the most of time out of training and the flexibility that allows.
Any other adventures along the way? Plenty! Lots of additional travelling, getting myself into and out of some ridiculous situations, and just generally having the ability to say yes rather than ‘let me check my rota’.
Any regrets? None
What are your plans now? Trying to maintain my involvement in Global Health while completing my Anaesthesia training. Then, who knows…..?
Can I be adventurous with medicine without taking time out?
For various reasons, time out from training might not be for everyone. Albeit often a little constrictive in terms of timings, with a little imagination and forward planning, it is possible to develop a keen interest in expedition and event medicine without taking ‘formal’ time out.
Some lucky few have managed to be granted study leave by training programme directors and educational supervisors. The skills you develop are easily applicable to any training pathway although some lend themselves to this better, notably ED and GP. Make sure your personal development plan includes pre-hospital/remote work and you show how the experience will benefit you as a trainee and the NHS in due course. For them to grant you this leave you will need to be achieving all of your competencies, be ahead with your portfolio and show you know what you are taking on.
Most still use annual leave for expeditions as it requires less hoop jumping. Aiming for one-two trips per year has been feasible for some of the team at AM. Booking leave with rota coordinators months in advance can be tricky, particularly if it’s for a future department you aren’t even working in yet. Try to make contact early and get the dates saved – you can always look to convert it to study leave later on.
Dream big but be realistic with how much you can take on. Shorter trips may be approved more easily and fit better with even the tightest of rotas. There are also numerous companies you can work for providing medical cover at 1-2 day events.
Adventure Medic’s Top Tips for Taking Time Out
- Plan early and be organised. Taking time out of training is becoming increasingly popular, and jobs (especially in Australia and NZ) are becoming more competitive.
- Research your options carefully, there are lots of opportunities out there, pick the right one to suit your personality/skill set/aspirations. Be aware that for many other countries, the working year doesn’t necessarily run August-August as it does in the UK.
- Also remember to plan carefully for your return to the UK. If you’re taking one year out, you’ll need to factor in time-off and money to return to the UK for interviews/assessments. Many people prefer to take two years out for just that reason. It is a shame to travel halfway around the world to work, but then have to spend all your annual leave travelling back to the UK for applications instead of exploring the country.
- Think about the financial implications of going away. The implications may be very good, if you are working in New Zealand or Australia. However, if you are going elsewhere, think about how you’ll pay your credit card/student loan/mortgage. Students loans need to be paid by direct debit while you are away. These can be frustrating to set up, as you need to give them an assessment of your projected income.
- If you plan on doing some locum work in the UK to help fund your travels, most health boards have a ‘Staff Bank’ – register with them for internal locuming opportunities. There are also many national locum agencies: Medacs, Reed Doctor etc . Be aware the registration process involves a lot of paperwork and can take many weeks – start early.
- Maintain your GMC registration whilst you are away. This may well be a pre-requisite e.g. for any expedition medic work, or for employment abroad. If you’re not doing clinical work, there is the option for ‘voluntary erasure’, but you then face quite a lot of paperwork and hassle to get re-registered on your return to the UK. There is also the option to stay on the register but relinquish your licence to practice. This may be the best option for anyone working abroad long term with a license with another country’s council. Just ensure that they’ll cover you for any extra work you do such as events/expeditions. If you’re not sure what to do, clarify the requirements of your overseas employer and talk it through with the GMC. If you do anything but keep your license, ensure you apply for it back in plenty of time for UK job applications.
- On completing Foundation Training you are awarded a Foundation Programme Completion certificate (FPCC) – this is mandatory for being accepted onto a Core or Specialty training programme and is valid for 3.5 years only. If you’re taking longer than 3.5 years out, you’ll need to provide formal evidence that your foundation competencies are up to date by getting a Consultant who has supervised you for at least 3 months to fill in an ‘Alternative Certificate’ for you. More information can be found on any of the Deanery websites.
- If you plan to return to the UK for further training, check the Person Specification for the Specialty Training programme you hope to apply for. This lists all the criteria and characteristics the admissions panel are looking for in their prospective trainees. Importantly, make sure you don’t end up with too much experience in a particular specialty to be eligible for entry-level training. Most specialties have an upper limit of around 18-24 months experience, any more and you may be forced to apply for jobs higher up the training scale e.g. ST3 and above.
- With GMC revalidation, it may pay off to collect a paper trail of references/supervisor reports/work-based assessments/multi-source feedback as you go along – it can only make your life easier in the long run. If working abroad, this may be an easy process to formalise by using their eportfolio e.g. ‘Inpractice’ in New Zealand.
- Be aware that on your job application you will have to give a full employment history, which involves justifying any gaps in employment of four weeks or longer. This is largely for probity/occupational health reasons, to ensure that you weren’t, for example, in a Thai jail. It is unlikely to cause you any penalty on your application, so do not let it put you off taking time time off for travelling, just be aware that you will have to explain the time away.
- If you’re planning on working in a developing world hospital or clinic, try to find out as much as possible about what you’re taking on before you go. Many doctors find themselves in at the deep end on arrival, which may pose difficult professional and ethical dilemmas. Speak to others who’ve been before, try to elicit what will be expected of you, and be explicit about your skill level and scope of practice.
- In checking the Person Specification, you may also be pleasantly surprised to see that there’s actually no scope for discriminating against you for taking time out. Try not to be put off by the fearmongering. In fact, you will more likely give yourself opportunity to acquire more application points through further relevant experience/demonstration of commitment to specialty/further audits & research.
- Finally, when you are back be sure to pen an article detailing your adventures for our esteemed publication. We look forward to reading all about it.
Useful links
We have a comprehensive list of links in our Resources Section but these are some to get you started.
- What to consider / A brilliant resource published by the British Medical Association, guiding you through every step of the process in taking time out to work and train in a developing country.
- BMA Guide to Working Abroad / Provides some country-specific guidance for working in NZ/Australia/North America/the EU as well as more general guidance for working in the developing world.
- NHS Medical Careers website: Medical Training Abroad / This is a thoughtful and well laid-out NHS resource for anyone considering taking time out of training to work abroad, or for those considering alternatives to practising NHS medicine. It also includes interesting case studies. Well worth a browse.
- GMC Guidance for taking time out of training / A useful resource published by the British Medical Association, explaining your medical registration and license options.
- BMA guide to time Out-Of-Programme (OOP) / Many ST programmes offer this, but your proposal must be approved by your Local Education and Training Board (LETB) in order for you to retain your national training number. The GMC also provides step-by-step guidance on arranging these.
- Certificate of Good Standing / You need one of these to register with an overseas regulatory body.
- Specialty Training Person Specifications / Outlining the criteria and competencies for selection for all Core and Specialty Training programmes.
- When adventure comes before ambition / The BMA News interviews Expedition and Wilderness Medicine’s Medical Director Amy Hughes on her eclectic path through medical training.







